Tailoring Therapies in Hormonal Imbalance
The human body is a symphony of hormones, each playing a delicate melody that dictates our health and well-being. When this orchestration goes awry, hormonal imbalances can ripple through our lives, causing a chorus of symptoms like fatigue, weight changes, mood swings, and even infertility. For decades, a one-size-fits-all approach has largely guided the treatment of these imbalances, often with suboptimal results.
But on the horizon gleams a revolution: personalized medicine, where therapies are meticulously crafted to fit the unique nuances of each individual’s hormonal fingerprint.
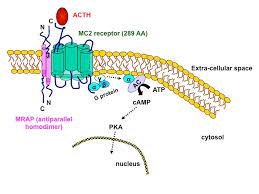
At the heart of this revolution lies ACTH, or adrenocorticotropic hormone. Produced by the pituitary gland, ACTH acts as a conductor, stimulating the adrenal glands to churn out cortisol, a hormone crucial for stress response, energy metabolism, and immune function. Understanding ACTH’s individual variations and their implications for hormonal imbalances is key to unlocking the promise of personalized medicine.
The Personalized Palette of ACTH:
ACTH, much like our personalities, is not a uniform entity. Genetic predispositions, environmental factors, and even lifestyle choices can paint a diverse palette of ACTH levels and responsiveness. Some individuals may naturally have higher or lower ACTH, while others may exhibit blunted or exaggerated responses to stimuli like stress or inflammation. These variations, in turn, can manifest as a spectrum of hormonal imbalances, each demanding a bespoke therapeutic approach.
For instance
Individuals with chronically elevated ACTH, often due to adrenal insufficiency or pituitary dysfunction, face an onslaught of cortisol, leading to symptoms like weight gain, muscle weakness, and high blood pressure. In such cases, the standard treatment of glucocorticoid replacement needs precise tailoring to match the individual’s unique ACTH levels and cortisol needs. Over-replacement can exacerbate existing problems, while under-replacement leaves the body vulnerable to stress and illness.
On the other end of the spectrum, those with ACTH deficiency experience the opposite, with cortisol production lagging behind. This can lead to fatigue, dizziness, and difficulty handling stress. For them, replacing cortisol in the precise dosage and form best suited to their individual ACTH dynamics is crucial for restoring balance and alleviating symptoms.
Moreover, personalized medicine takes a deeper dive into the underlying causes of these imbalances. Genetic testing can reveal predispositions to specific hormonal vulnerabilities, allowing for preventive interventions or early detection of potential problems. Similarly, advanced biochemical analyses can unveil subtle variations in individual hormone metabolism, guiding the selection of the most effective and targeted treatments.
Beyond Cortisol: A Wider Orchestral Perspective:
The magic of personalized medicine extends beyond simply tuning the cortisol dial. ACTH’s influence cascades down the hormonal hierarchy, impacting the production and activity of other crucial players like thyroid hormones, sex hormones, and insulin. Understanding how these hormones interact in the individual’s unique symphony is crucial for crafting truly comprehensive therapies.
For example, a woman with polycystic ovary syndrome (PCOS) may have elevated ACTH due to chronic stress, which in turn disrupts her insulin and androgen levels, contributing to fertility issues and metabolic problems. In such a case, personalized treatment would not only address the ACTH-cortisol imbalance but also consider interventions to regulate insulin and androgen activity, potentially unlocking a more holistic approach to managing PCOS.
The Future Symphony: Precision, Prediction, and Prevention:
The future of personalized medicine in hormonal imbalances paints a vibrant picture. Advanced AI algorithms will analyze complex datasets of genetic, biochemical, and clinical data to predict individual vulnerabilities and tailor treatment plans with unprecedented precision. Imagine a world where hormonal imbalances are not reactive diagnoses but proactively prevented, thanks to tailored lifestyle modifications and early interventions based on each person’s unique hormonal blueprint.
The journey towards this future requires continued research to unravel the intricate tapestry of ACTH and its downstream effects. But the potential rewards are immense: empowered individuals, thriving communities, and a healthcare system that resonates with the unique melody of each human life.
-
The Nuances of ACTH Testing:
Understanding individual ACTH levels is crucial for personalized therapy. Beyond routine blood tests, specialized tests like the cosyntropin stimulation test and low-dose dexamethasone suppression test assess the pituitary gland’s ability to produce ACTH and the adrenal glands’ responsiveness to stimulation. Additionally, salivary cortisol testing offers a glimpse into the body’s “free” cortisol, providing a more accurate picture of the biologically active hormone available to tissues.
-
Beyond Cortisol: The Hormonal Entourage:
As mentioned earlier, ACTH orchestrates a complex hormonal ensemble. Examining levels of hormones like DHEA, thyroid hormones, sex hormones, and insulin alongside cortisol paints a more complete picture of the imbalance. For example, in Cushing’s syndrome, elevated ACTH leads to high cortisol and DHEA, often alongside low thyroid hormones and sex hormones. Tailoring therapy to address all these imbalances, not just cortisol, is key to managing the condition effectively.
-
Precision Therapy: From Bench to Bedside:
Personalized medicine translates research findings into actionable treatment plans. For instance, genetic testing can reveal mutations in genes related to cortisol metabolism, guiding therapy choices. Similarly, pharmacogenetic testing can predict individual responses to specific medications, allowing for the selection of drugs with optimal efficacy and minimal side effects.
Case Studies: The Melody of Individuality:
To illustrate the power of personalized ACTH therapy, consider these scenarios:
- Maria, the Stressed Musician: Chronically elevated ACTH due to performance anxiety disrupts Maria’s sleep, metabolism, and mood. By understanding her unique ACTH response to stress, her doctor can recommend targeted stress management techniques like cognitive-behavioral therapy alongside carefully modulated cortisol replacement therapy.
- Tom, the Athlete with Adrenal Insufficiency: Intense training depletes Tom’s already low adrenocortical reserves, leading to fatigue and decreased performance. Personalized dosing of cortisol replacement helps him optimize his energy levels and training without triggering side effects.
- Ava, the PCOS Puzzle: Ava’s elevated ACTH contributes to her PCOS symptoms like acne and irregular periods. However, genetic testing reveals a specific insulin resistance-related mutation. By addressing both the ACTH-cortisol axis and insulin sensitivity, her doctor crafts a personalized approach that alleviates her symptoms and improves her fertility prospects.
Embracing the Future Symphony:
The integration of ACTH into personalized medicine represents a paradigm shift in treating hormonal imbalances. By deciphering the individual hormonal language, we can craft therapies that resonate with each unique bio-melody. This precision not only promises improved symptom management but also opens doors for preventative interventions and personalized wellness strategies.
As research continues to unlock the secrets of the ACTH concerto, the future of personalized hormone therapy becomes increasingly clear: a future where healthcare becomes a tailor-made symphony, conducted by the maestro of individual needs, and harmonizing the delicate balance of hormones within each of us.
Additional Notes:
- This expanded version further explores the nuances of ACTH testing, the concept of the hormonal entourage, and the application of precision therapy in specific cases.
- It emphasizes the personalized nature of treatment and the future potential of preventative interventions based on individual hormonal profiles.
Can Pheromones Influence Human Behavior and.
The concept of pheromones, chemical substances that play a crucial role in communication among animals, has long intrigued scientists and.
Read Morehow growth hormone helps in height.
Growth hormone (GH), a vital hormone produced by the pituitary gland, plays a crucial role in physical growth and development..
Read More