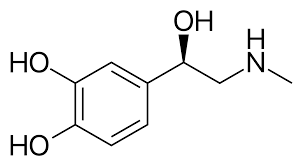
In the intricate ballet of hormones (Adrenaline), a mischievous imposter lurks, masked as the king of stress, cortisol. This phantom performer – an epinephrine mimic – orchestrates a deceptive play called hypercortisolism, mimicking the symptoms of Cushing’s Syndrome while leaving the true culprit, the adrenal glands, unscathed. Unmasking this imposter is a medical detective story, a thrilling pursuit through the labyrinth of symptoms and tests, with the well-being of the patient hanging in the balance.
Cushing’s Syndrome: The True King of Cortisol Chaos:
Cushing’s Syndrome, the genuine ruler of hypercortisolism, arises from an overproduction of cortisol by the adrenal glands, often due to a tumor or medication use. This hormonal excess throws the body’s orchestra into disarray, manifesting in weight gain, muscle weakness, high blood pressure, and other debilitating symptoms.
Enter the Epinephrine Understudy:
But sometimes, a cunning understudy, an epinephrine mimic, steals the spotlight. These imposters, often medications or medical conditions, trick the body’s receptors into responding as if they were witnessing true, cortisol-driven hypercortisolism. It’s like watching a masterfully crafted production where the set, costumes, and even the script resemble the original, yet something feels subtly off.
The Masquerade of Mimics:
The masquerading culprits are diverse, each playing their part in this hormonal deceit:
- Beta-agonists: Used for asthma and heart conditions, these medications can stimulate cortisol receptors, leading to weight gain, high blood pressure, and other Cushingoid features.
- Tricyclic antidepressants: While effective in treating depression, they can also trigger cortisol-like effects, potentially masking or mimicking true Cushing’s Syndrome.
- Licorice: Surprisingly, even this seemingly innocent treat can fool the body’s hormonal receptors, causing temporary hypertension and other symptoms reminiscent of Cushing’s.
- Severe stress: In extreme cases, chronic stress can drive up cortisol levels, creating a temporary hypercortisolism-like picture that requires careful differentiation from the true syndrome.
The Detective’s Dilemma:
Diagnosing true Cushing’s Syndrome becomes a delicate dance of discerning truth from fiction. Doctors must become medical detectives, scrutinizing every clue and employing an array of tests to unmask the imposter:
- Cortisol Levels: While elevated cortisol levels are suggestive, they can also occur in a multitude of conditions, necessitating further investigation.
- Low-dose dexamethasone suppression test: This test is a key player, as a blunted response to dexamethasone suggests true Cushing’s Syndrome, while normal suppression points away from it.
- Midnight salivary cortisol: Measuring cortisol levels at night offers another valuable piece of the puzzle, as nighttime levels should be low in healthy individuals but remain elevated in Cushing’s Syndrome.
- Imaging tests: CT scans, MRIs, and PET scans can help visualize potential adrenal tumors or other structural abnormalities that might be the source of the excess cortisol production.
Unmasking the Imposter:
The detective work, though meticulously thorough, can be challenging. Epinephrine mimics are skilled deceivers, and their effects can overlap significantly with true Cushing’s Syndrome. Careful analysis of medical history, medication use, and the nuances of symptoms is crucial to unveil the truth.
Treatment: Tailoring the Response:
Once the mask is torn off and the imposter identified, the treatment course diverges dramatically. For true Cushing’s Syndrome, addressing the underlying cause, whether it’s a tumor or medication, is paramount. Surgery, radiation therapy, or targeted medications might be required to bring cortisol levels back in line.
However, for epinephrine mimics, the focus shifts to stopping the source of the masquerade. Discontinuing the offending medication, managing stress effectively, or finding alternative treatment options become the keys to restoring hormonal balance and alleviating the masquerade of symptoms.
Beyond the Diagnosis (Adrenaline):
The journey doesn’t end with unmasking the culprit. The emotional toll of a misdiagnosis can be significant, with the uncertainty and invasive tests leaving patients feeling vulnerable and frustrated. Therefore, providing ongoing support and addressing the psychological impact of this medical detective story is equally important.
The Epinephrine Enigma:
The existence of epinephrine mimics exposes the intricate web of communication between hormones and their receptors. It serves as a reminder that diagnosis, especially in complex cases, is not a linear process but a nuanced puzzle where careful reasoning and thorough investigation are paramount-Adrenaline
While the masquerade of hypercortisolism can be daunting, the power lies in unraveling the deception. By understanding the tricks of the epinephrine mimics and employing rigorous diagnostic tools, we can empower medical detectives to unmask the imposters and ensure the well-being of those trapped in this hormonal play.
Cushing’s Syndrome: The Genuine Maestro’s Meltdown:
When the adrenal glands, our hormonal opera house, churn out excessive cortisol, a genuine case of Cushing’s Syndrome unfolds. This hormonal overture plays havoc on the body’s orchestra, manifesting in weight gain, moon-shaped face, thinning limbs, and a crescendo of other debilitating melodies.
Epinephrine’s Understudy Takes the Stage:
But sometimes, the conductor’s spotlight falls upon an imposter. Epinephrine mimics, cunning actors in the hormonal play, hijack cortisol receptors, triggering a deceptive performance of hypercortisolism. The stage is set with familiar symptoms: weight gain, muscle weakness, high blood pressure – a chilling echo of the genuine condition, yet subtly off-key.
The Masquerade of Malefactors:
The cast of these hormonal imposters is diverse, each playing their part in the deceptive play:
- Beta-agonists: These medications for asthma and heart conditions, like mischievous understudies, strut onto the stage, mimicking cortisol’s effects on receptors, leading to weight gain, hypertension, and bone loss.
- Tricyclic antidepressants: While effective in combating depression, they too can don the cortisol mask, triggering similar symptoms, further muddying the diagnostic waters.
- Licorice: This seemingly innocent treat harbors a surprising secret. High doses of licorice can trick the body’s receptors, causing temporary hypertension and mimicking the moon-shaped face of Cushing’s Syndrome.
- Severe stress: In the face of chronic stress, our bodies can crank up cortisol production, leading to a temporary hypercortisolism-like picture, demanding careful differentiation from the true syndrome.
The Medical Detective on the Hunt:
Diagnosing true Cushing’s Syndrome becomes a forensic investigation, a hunt for clues amidst the cacophony of symptoms. Doctors, transformed into medical detectives, scrutinize every detail, employing an array of tests to unmask the impostor:
- Cortisol Levels: While elevated cortisol levels raise suspicion, they can also be the whispers of other conditions, necessitating further sleuthing.
- Low-dose Dexamethasone Suppression Test: This crucial test acts as a lie detector, exposing the imposter. A blunted response to dexamethasone points towards the culprit, while normal suppression clears the understudy’s name.
- Midnight Salivary Cortisol: Measuring cortisol levels at night paints a clearer picture. In healthy individuals, these levels should be low, while in true Cushing’s, they remain elevated, like a persistent murmur in the hormonal symphony.
- Imaging Tests: Like CSI agents scanning for evidence, CT scans, MRIs, and PET scans can unveil potential adrenal tumors or other structural clues that might point to the true source of the hormonal imbalance.
Adrenaline-Unmasking the Deception
The detective work demands meticulousness. Epinephrine mimics are skilled actors, their performances eerily similar to the genuine Cushing’s Syndrome. Analyzing medical history, medication use, and the nuanced tapestry of symptoms becomes crucial to expose the true culprit.
Tailoring the Treatment to the Tune:
Once the mask is ripped off, the treatment script rewrites itself. For true Cushing’s Syndrome, quelling the rebellious adrenal glands takes center stage. Surgery, radiation therapy, or targeted medications become the tools to silence the overzealous conductor and restore hormonal harmony.
However, for epinephrine mimics, the focus shifts to stopping the masquerade at its source. Discontinuing the offending medication, managing stress effectively, or finding alternative treatment options become the melodies that restore balance and silence the deceptive tune of the imposters.
Beyond the Diagnosis: The Aftershocks of Deception:
The journey doesn’t end with the culprit unmasked. The emotional toll of a misdiagnosis can linger, a discordant note in the aftermath of the medical drama. The uncertainty and invasive tests can leave patients feeling vulnerable and frustrated. Therefore, providing ongoing support and addressing the psychological impact of this medical detective story is equally important.
Epinephrine’s Enigma: A Symphony of Caution:
The existence of epinephrine mimics exposes the intricate web of communication between hormones and their receptors. It serves as a stark reminder that diagnosis, especially in complex cases, is not a simple melody but a nuanced symphony where careful reasoning
